Advanced Pain Management Techniques
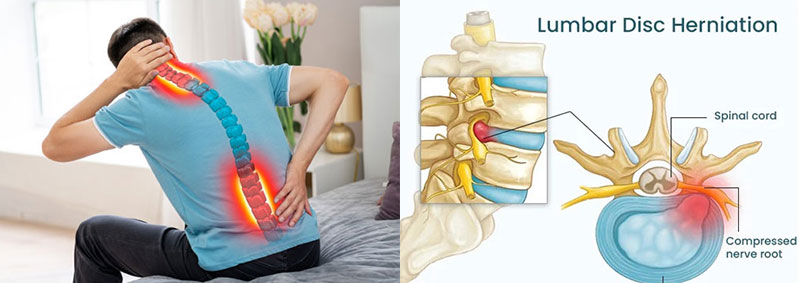
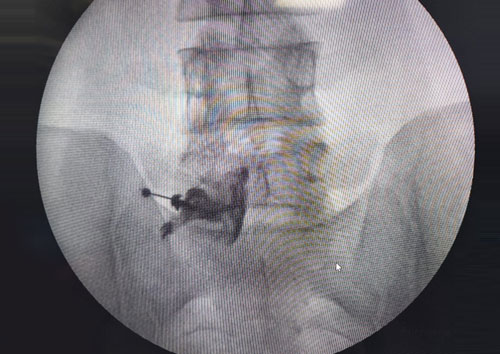
1. Selective Nerve Root Block for Lumbar Disc Prolapse
Selective nerve root blocks are a vital tool for diagnosing and treating lumbar disc prolapse. This procedure involves injecting anesthetic and, when appropriate, corticosteroids near the affected nerve root. By targeting specific areas, we can alleviate pain caused by nerve compression and reduce inflammation, providing both immediate relief and valuable diagnostic information.
Key Benefits:
- Effective pain relief for radiculopathy
- Reduced inflammation and irritation
- Enhanced mobility and daily function
- Clearer diagnosis of pain sources
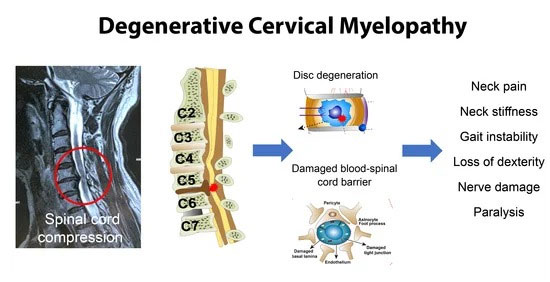
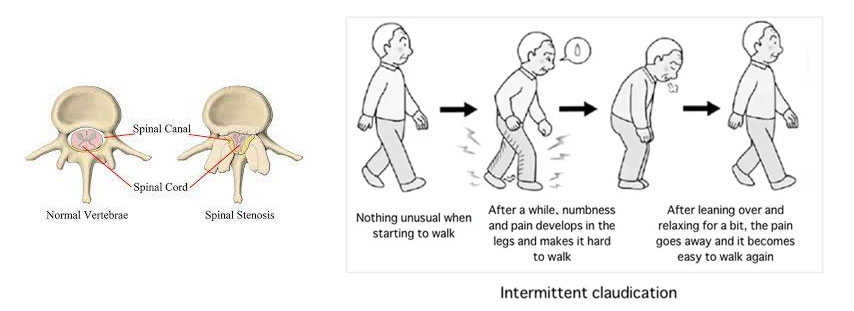
2. Cervical Epidural Injections
Cervical epidural injections deliver medication directly into the epidural space of the cervical spine, effectively treating conditions like herniated discs, cervical spondylosis, and spinal stenosis. This minimally invasive procedure targets inflammation around the spinal cord and nerve roots, offering significant pain relief and improved functionality.
Key Benefits:
- Targeted and effective pain management
- Minimally invasive with quick recovery
- Potential to delay or avoid surgical intervention
- Comprehensive approach to neck pain relief
3. Facet Joint Blocks
Facet joint blocks involve injecting anesthetic into the facet joints of the spine to alleviate pain associated with arthritis or injury. This procedure not only provides immediate pain relief but also assists in identifying the source of discomfort, allowing for a more tailored treatment plan.
Key Benefits:
- Direct targeting of facet joint pain
- Immediate and lasting pain relief
- Enhances diagnostic accuracy
- Supports comprehensive treatment strategies
4. Ganglion Impar Block for Coccydynia
For patients suffering from coccydynia (tailbone pain), the ganglion impar block offers targeted relief. This procedure involves injecting anesthetic near the ganglion impar, effectively interrupting pain signals and alleviating discomfort. Ideal for those who have not responded to conservative treatments, this block can significantly improve quality of life.
Key Benefits:
- Direct relief for coccydynia
- Minimally invasive with low recovery time
- Effective in reducing pain and discomfort
- Can enhance overall mobility and function